The Future of Prior Authorization
By: Kevin Narine and Christopher Sanfilippo, Forum Systems
Prior Authorization has long been a pain point for providers. Sometimes called prior auth or just PA, it means, put simply, certain treatments must be authorized by an insurer before they are administered.
Prior Authorizations are sent by providers and reviewed by payers who then authorize or decline the request. The payer may also direct the provider to a more cost-effective treatment, such as using generic over brand-name drugs. Prior authorization exists to ensure that the recommended treatment is both necessary and will be effective—and to eliminate superfluous costs.
The 2021 American Medical Association Prior Authorization Physician Survey reported some alarming figures: A full 82% of physicians report that treatment has been abandoned owing to the onerous PA process. Even worse, 8% of physicians report that PA delays have “led to a patient’s disability/permanent bodily damage, congenital anomaly/birth defect or death.” The opinion of doctors is clear: something needs to be done.
Even as the healthcare industry moves toward value-based care (as opposed to fee-for-service), prior authorization will remain, especially insofar as it promotes evidence-based care, safety, and affordability. The question is not how to get rid of prior authorization but rather how it can be optimized and automated. How can prior authorization work for patients, providers, and payers?
Electronic Prior Authorization Workflows
The principal way in which prior authorization—the most expensive and time-consuming transaction to do by hand—will be improved is by broad adoption of a fully or mostly electronic prior authorization workflow that implements nationally recognized standards. Such a workflow is sometimes called electronic prior authorization or ePA.
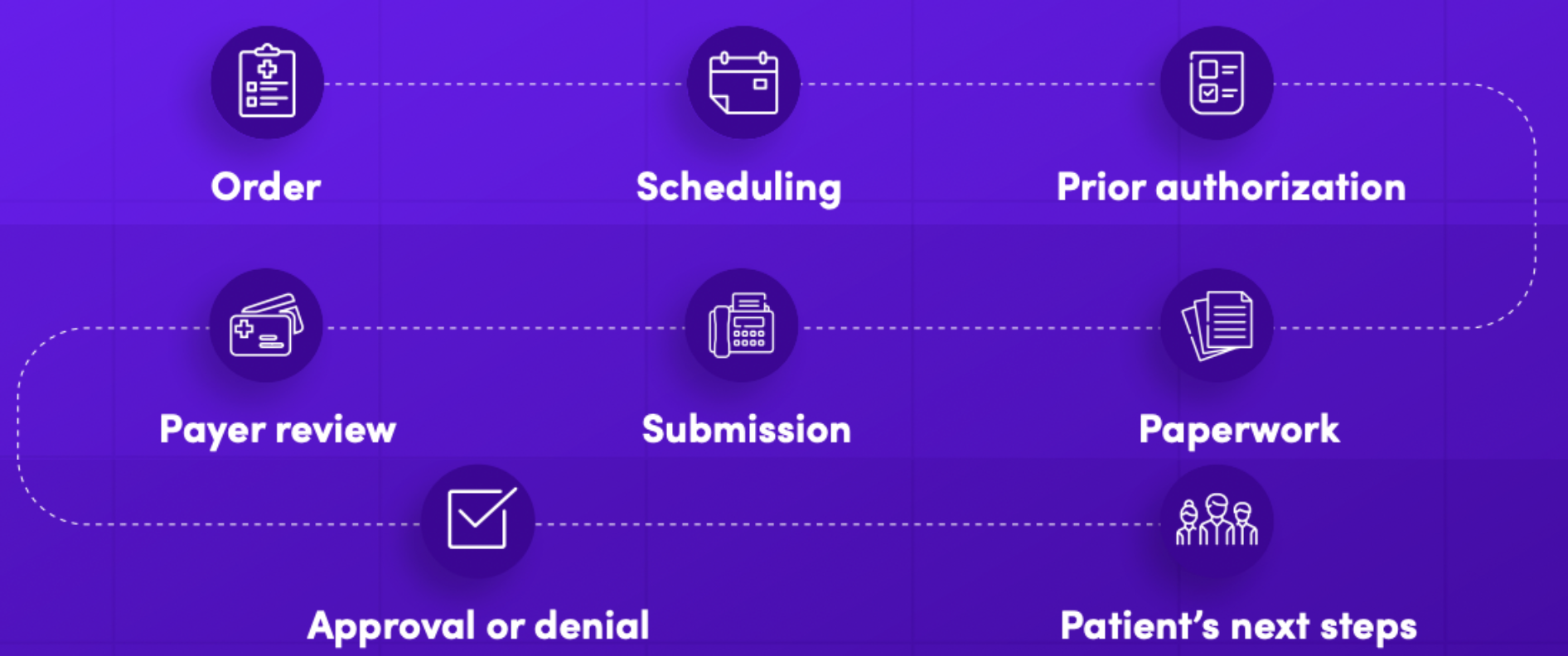
Such a workflow would begin with a request submitted through an online portal. That request would communicate with the patient’s EMR to automatically include relevant case and clinical data. It could also electronically include relevant attachments (as long as Transaction Set 275 is supported). The EMR software would review the request to ensure completeness, then forward it to the payer. The payer’s software would again automatically review the request—and it may even be approved within one day if everything is in order. Or, the request may be flagged because, for example, it requires further documentation, which again can be requested and submitted through an online portal instead of being faxed. And the provider can observe the status of the request at each stage in the process. In the final step, the payer would either approve or deny the request.
The two main electronic standards are X12 EDI (Transaction Set 278 for PA) and FHIR (Fast Healthcare Interoperability Resource). FHIR—being HTTP- and API-based—appears to be the favored standard for the future. For example, a new CMS ruling (Interoperability and Patient Access Final Rule) mandates FHIR. But more important is the transition itself to ePA.
The 2021 CAQH Index, which tracks the digitization of healthcare, reports low numbers for the adoption of ePA: 26% fully and 39% partially electronic—leaving a whole 35% still fully manual that rely on hand-filled paper documents, faxes, and telephone calls. In 2019, CAQH estimated the industry could save $454 million per year by switching to fully electronic prior authorization. The most recent estimate from 2021 remains a staggering $437 million in potential savings. In real terms, 16 minutes per transaction could be saved. With 142 million prior authorization transactions happening per year, the scale of inefficiency is enormous.
Coming Changes to Prior Authorization
Several organizations promote the adoption of HL7 FHIR standards; leading the charge is the Da Vinci Project whose stakeholders “are industry leaders and health IT technical experts who are working together to accelerate the adoption of [HL7 FHIR] as the standard to support and integrate value-based care (VBC) data exchange across communities.” They have written a helpful guide ePA Implementation Guide.
Major changes are coming that will all but require the transition to electronic prior authorization. Last year, CAQH CORE—a group of private and governmental healthcare organizations which together cover about 3/4 of all commercially insured lives—announced a two-day limit for health plans to respond to prior authorization requests. And the recent No Surprises Act touches on prior authorization as well: emergency treatments, even those administered out-of-network, will no longer require prior authorization, but plans will be required to spell out in advanced explanations of benefits (EOBs) which treatments will require prior authorization.
The future of healthcare is digital—about this there can be no doubt. Every organization within the healthcare ecosystem needs to prepare for this transformation. The adoption of electronic prior authorization is a crucial step toward bringing healthcare into the 21st century.
Recommendations
As with any strategic endeavor, health organizations must identify their current choke points to see how their workflows can improve. Forum Systems recommends:
- Assess your current prior authorization workflow for pain points
- Engage healthcare technology experts—such as Forum Systems—who can assess your current capacities and advise on and oversee your adoption of an interoperable and compliant electronic prior authorization process
- Develop a plan to integrate new prior authorization workflows and assess their impact, as well as a feedback mechanism for iterative improvement
About Forum Systems
Forum Systems is a leader in intelligent API gateway technology, deep data analytics and cloud technologies. Forum technology, used by some of the largest global companies for building intelligent business workflows, is certified and secure. Along with industry-leading performance, interoperability, and security, Forum Systems takes pride in their customer-driven innovation and simplified user experience.